At Houston Methodist, the operating room sits at the center of both patient care and financial performance. As margins tighten and labor costs rise, leadership has sharpened its focus on getting more from existing OR capacity.
Yet, despite ongoing efficiency initiatives and experienced teams, many surgical days still unraveled by midday. Cases often ran shorter or longer than expected, staffing adjustments accumulated, and confidence in the schedule steadily eroded. Over time, it became clear that the challenge wasn’t just managing the day as it unfolded — the schedule itself was setting teams up to fall behind.
Inaccurate case duration estimates meant the OR often started the day with a plan that didn’t reflect reality, making downstream inefficiencies almost inevitable.
When the schedule doesn’t match reality
Before Apella, case scheduling at Houston Methodist relied primarily on two inputs: EHR-based forecasts and surgeon estimates. EHR forecasts were based on limited historical data and failed to reflect real-world variability, while surgeon estimates were subjective and inconsistent. Neither captured the true complexity of the OR, including time-of-day patterns, surgeon-specific behaviors, or case sequencing effects. The downstream impact was significant:
- Underscheduled cases led to unplanned overtime
- Overscheduled cases left OR time unused
- Blind spots obscured which cases posed the greatest risk
- Eroding trust reduced confidence in the schedule
Inaccurate scheduling created cascading effects across staffing, anesthesia coverage, overtime costs, and OR flow.
Learn how Houston Methodist used Flagged Cases to cut late OR days in half.
Read the case study
Using ground-truth data to quantify the opportunity
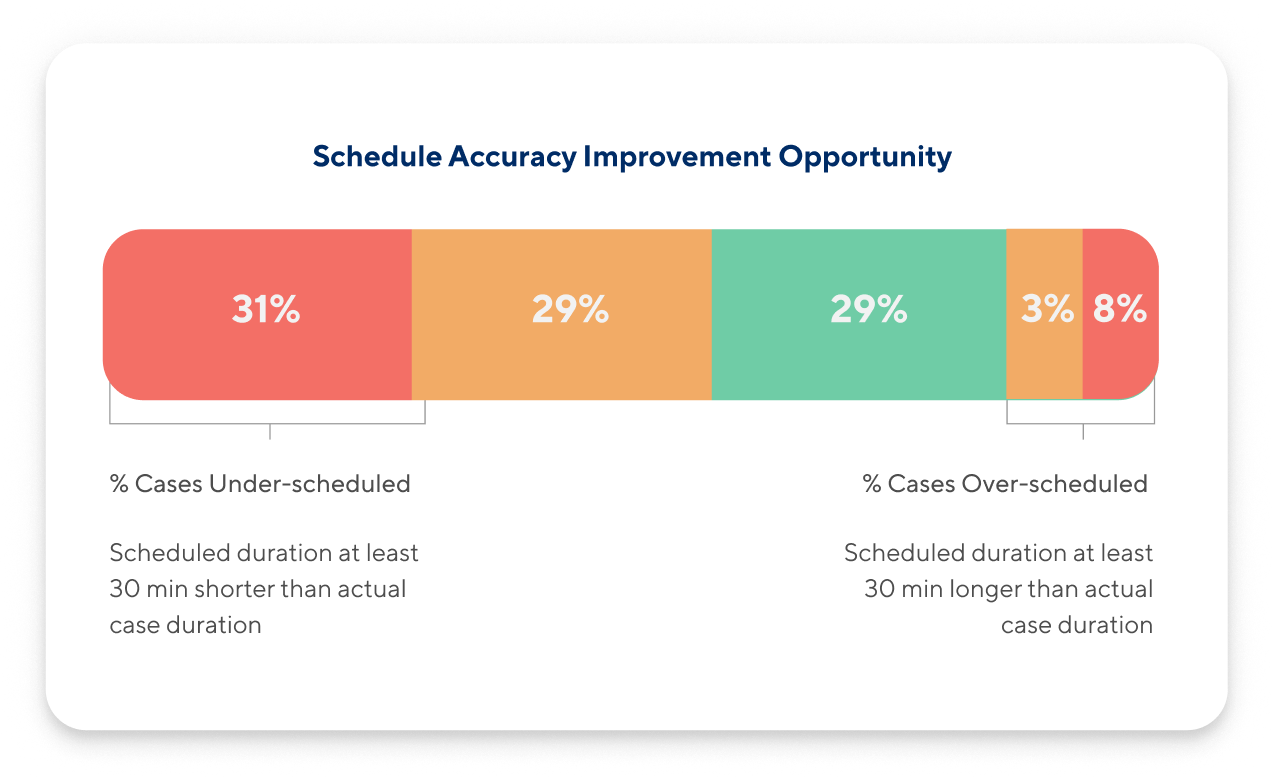
Houston Methodist turned to Apella to quantify the scheduling gap, comparing EHR-scheduled durations with Apella’s ground-truth observations across six sites.
The analysis revealed that only 29% of cases were scheduled within ±30 minutes, 60% were underscheduled by more than 30 minutes, and nearly 40% were off by more than an hour. The data confirmed that teams were often starting the day at a disadvantage.
Closing the gap with Flagged Cases
From May to July 2025, Houston Methodist ran an eight-week pilot of Apella’s Flagged Cases tool.
Powered by Apella’s ambient AI, Flagged Cases combines real-time OR activity with contextual factors — such as surgeon-specific patterns and case sequencing — to surface cases most likely to be significantly over- or underscheduled.
By prioritizing the cases with the greatest downstream impact, schedulers were able to focus their time where it mattered most. Instead of reviewing every case, they were able to easily identify the cases most likely to derail the day — achieving meaningful improvement with minimal workflow disruption.
Flagged Cases also provided an objective foundation for aligning schedulers, surgeons, and perioperative leaders around a shared source of truth.
Fewer late days, more accurate schedules
Within two months, Houston Methodist saw measurable improvements, without reducing case volume, on days where cases were flagged as over- or under-scheduled by Apella:
- 2.3x increase in accurately scheduled cases (29% to 68%)
- 73% decrease in proportion of underscheduled cases (60% to 16%)
- 69 fewer unplanned late minutes per OR on days with rescheduled cases
- 46-percentage-point reduction in late OR days flagged by Apella
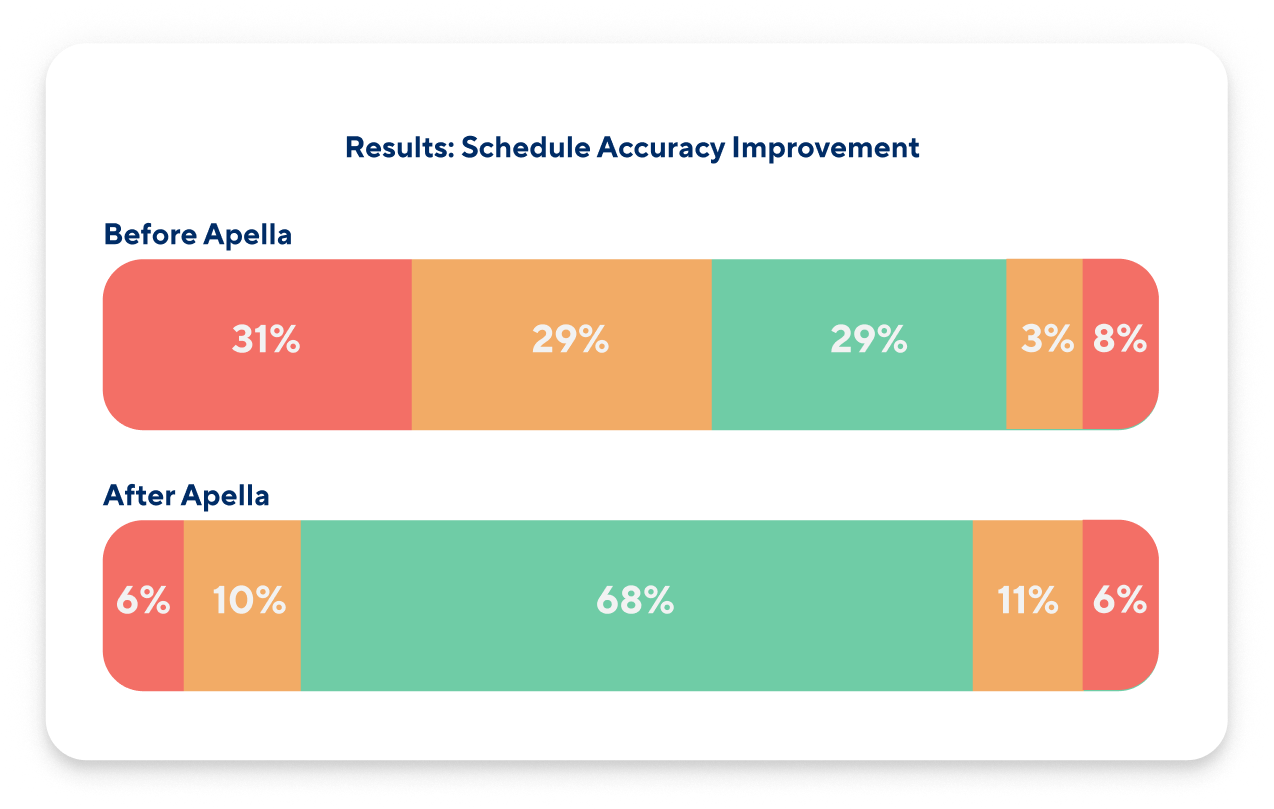
Improved scheduling accuracy translated directly into more predictable days, fewer late finishes, and better use of existing OR capacity.
A more predictable, collaborative OR
The pilot reinforced a critical takeaway: scheduling accuracy depends on the quality of the data behind it. By moving from subjective inputs to ground-truth observations, Houston Methodist is building a more predictable, collaborative, and scalable approach to OR operations.